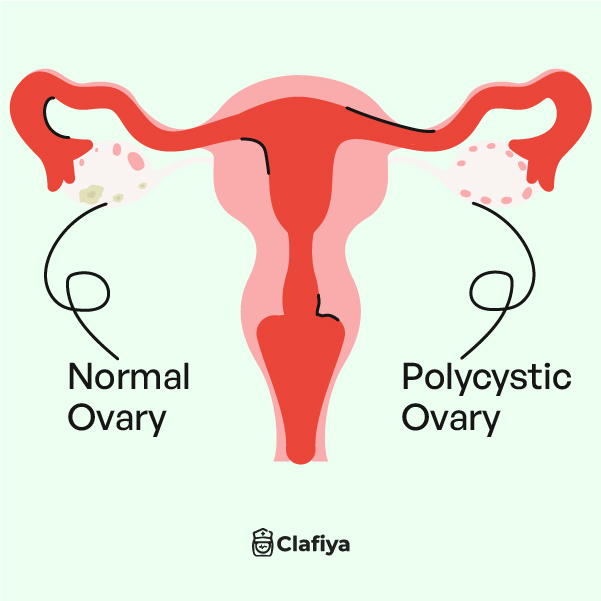
You’ve probably heard of PCOS, but what does it really mean? Polycystic Ovarian Syndrome (PCOS) is a condition that affects millions of women worldwide, yet it remains widely misunderstood. Whether you’re newly diagnosed or just looking to learn more about a recurring subject, this article will break down everything you need to know about PCOS in 2024 as a Nigerian woman, from its full meaning to the best treatments available.
What is the meaning of PCOS?
PCOS is short for Polycystic Ovarian Syndrome. It is a hormonal disorder that affects a woman’s hormone levels. Women with PCOS produce more amounts of male hormones than is considered normal.
The full meaning of PCOS is important to understand because it gives us insight into the condition’s core issues: ‘poly’ means many, ‘cystic’ refers to cysts, and ‘ovarian’ indicates that the problem is related to the ovaries. However, despite its name, not every woman with PCOS will develop ovarian cysts.
PCOS is primarily characterised by an imbalance of reproductive hormones called androgens, which can lead to a variety of symptoms and health complications. This condition is particularly concerning because it disrupts the cycle causes infertility in women, and it can also have long-term health effects if left untreated.
What causes PCOS?
The exact cause of Polycystic Ovarian Syndrome (PCOS) is still not fully understood. However, researchers believe it arises from genetic and environmental factors. If PCOS runs in your family or if there’s a history of diabetes or endocrine disorders, your chances of developing it might be higher. Let’s take a closer look at the potential causes of PCOS.
- Insulin resistance: One of the main factors linked to PCOS is insulin resistance. This happens when your body’s cells don’t respond properly to insulin, the hormone responsible for regulating blood sugar. As a result, your body produces more insulin, which can cause your ovaries to make more androgens (male hormones like testosterone). These elevated androgen levels are responsible for many PCOS symptoms, such as irregular periods and excess hair growth.
- Genetic factors: If you have a family history of PCOS or related conditions, such as diabetes or thyroid disorders, you may be more susceptible to developing PCOS. This suggests a genetic link, although specific genes haven’t been identified yet.
- Inflammation: Women with PCOS often have low-grade inflammation. This chronic inflammation can trigger the ovaries to produce more androgens, worsening symptoms and potentially contributing to insulin resistance.
These factors often work together to disrupt the normal balance of hormones in the body, leading to the development of PCOS. Understanding these causes is essential in managing and treating the condition effectively.
How do I know I have PCOS?
You may have been hearing about PCOS but you’re not sure if your symptoms apply. Recognising the symptoms of PCOS is super important for diagnosis and treatment. Here are some of the most common signs of PCOS:
- Irregular periods: One of the most common symptoms of PCOS is irregular menstrual cycles. This might mean fewer periods, more frequent periods, or very heavy periods.
- Excess hair growth: This condition is known as hirsutism. It is caused by elevated levels of androgens. Women with PCOS may notice hair growth on their face, chest, back, and other areas where men typically grow hair.
- Acne and oily skin: High androgen levels can also lead to acne, especially on the face, chest, and upper back.
- Weight gain: Many women with PCOS struggle with weight gain, particularly around the abdomen. This weight gain is often linked to insulin resistance.
- Thinning hair: While some women with PCOS experience excess hair growth, others may notice thinning hair on their scalp.
- Darkening of the skin: Patches of dark skin, particularly around the neck, under the breasts, and in the groin area, can be a sign of insulin resistance, which is often seen in PCOS.
- Polycystic ovaries: As the name suggests, women with PCOS may develop multiple small cysts on their ovaries. These cysts are actually immature follicles that have failed to release eggs.
How does PCOS affect the body?
PCOS can affect various aspects of your health, not just your reproductive system. Here’s a detailed look at how PCOS impacts different parts of your body:
- Reproductive system: PCOS is a leading cause of infertility because it disrupts the normal ovulation process. Women with PCOS may struggle to conceive due to irregular or absent ovulation.
- Metabolic health: PCOS significantly increases the risk of metabolic disorders. Women with PCOS are at a higher risk for developing type 2 diabetes, high blood pressure, and high cholesterol, all of which contribute to cardiovascular disease.
- Endocrine system: As mentioned earlier, PCOS is closely linked to insulin resistance, which can lead to prediabetes or type 2 diabetes. Insulin resistance also exacerbates weight gain, particularly in the abdominal area, which can be challenging to manage.
- Skin and hair: The high androgen levels in PCOS can lead to skin issues like acne and oily skin, as well as hirsutism. At the same time, some women may experience thinning hair or hair loss on the scalp, a condition known as androgenic alopecia.
- Mental health: PCOS can take a toll on your mental well-being. Many women with PCOS experience depression, anxiety, and mood swings. The physical symptoms of PCOS, such as weight gain and acne, can also lead to body image issues and lower self-esteem.
- Sleep: Women with PCOS are at a higher risk of developing sleep apnea, a condition where breathing repeatedly stops and starts during sleep. This is particularly true for women who are overweight or obese.
How can I get tested for PCOS?
If you suspect you have PCOS, getting tested is the first step toward understanding and managing your condition. Here’s what the testing process typically involves:
- Medical history and physical exam: Your healthcare provider will ask about your menstrual cycle, weight changes, and symptoms like excess hair growth and acne. They will also check your blood pressure, body mass index (BMI), and waist circumference.
- Blood tests: Blood tests are used to measure hormone levels, including androgens, insulin, and other reproductive hormones like LH (luteinizing hormone) and FSH (follicle-stimulating hormone). A blood sugar test may also be conducted to check for insulin resistance or diabetes.
- Pelvic exam: During a pelvic exam, your doctor will check for any abnormalities in your reproductive organs, including your ovaries.
- Ultrasound: An ultrasound is often used to look at your ovaries and uterus. This imaging test can show the presence of cysts on the ovaries and measure the thickness of the uterine lining.
- Other tests: In some cases, additional tests like a glucose tolerance test or lipid profile may be recommended to assess your risk for diabetes and heart disease.
PCOS can feel overwhelming, but you don’t have to go through this alone. At Clafiya’s Care Clinic, you can get tested for PCOS with compassionate care and support from our dedicated health professionals anywhere in Nigeria.
We’ll guide you every step of the way to help you understand your diagnosis and find the right treatment plan.
How is PCOS treated?
PCOS, or Polycystic Ovarian Syndrome, is a chronic condition, but the good news is that its symptoms can be managed. While there’s no cure for PCOS, a combination of treatments can help improve your quality of life and reduce complications. These treatments typically fall into four main categories: medication, surgery, diet, and lifestyle changes. Here’s everything you need to know about treating PCOS, especially as we recognize PCOS Awareness Month 2024.
Medication:
Medications are often the first line of treatment for Polycystic Ovarian Syndrome, aimed at regulating hormones, managing insulin levels, and alleviating specific symptoms such as irregular periods or acne. If you’re wondering, “Can PCOS be treated?”, the answer is yes—with medication being a major factor.
- Birth control pills: These are commonly prescribed to regulate menstrual cycles, reduce androgen levels, and control symptoms like acne and excess hair growth.
- Metformin: This medication is often used to treat insulin resistance and lower blood sugar levels in women with PCOS.
- Anti-androgens: These medications, such as spironolactone, can help reduce excess hair growth and other symptoms caused by high androgen levels.
- Fertility medications: If you’re trying to conceive, your doctor may prescribe medications like clomiphene or letrozole to stimulate ovulation.
Surgery:
In certain cases, surgery may be recommended for women with PCOS, particularly if other treatments haven’t been effective. While surgery is not typically the first option, it’s often considered when weighing PCOS vs endometriosis, especially for fertility improvement.
- Ovarian drilling: In cases where medication isn’t effective, a surgical procedure called ovarian drilling may be recommended. This procedure involves making small holes in the ovary using a laser or thin needle heated with an electric current. It can help restore regular ovulation.
- Hysterectomy: However, if you’re asking, “Will a hysterectomy cure PCOS?”, it’s important to know that while it may alleviate symptoms, it’s not considered a cure for PCOS. A hysterectomy, the removal of the uterus, may be considered if there are other serious health issues like endometrial cancer, but it does not address the root causes of PCOS.
Diet and lifestyle changes:
Lifestyle adjustments, such as regular exercise and stress management, are essential for managing PCOS. Some changes include:
- Weight management: Losing even a small amount of weight can help regulate your menstrual cycle and improve symptoms of PCOS. A balanced diet rich in whole foods, vegetables, lean proteins, and healthy fats is key.
- Exercise: Regular physical activity can help manage weight, improve insulin sensitivity, and reduce the risk of cardiovascular disease.
- Supplements: You might also explore the best supplements for PCOS, such as inositol or vitamin D, which can help regulate blood sugar and hormone levels. These can help improve insulin resistance, reduce inflammation, and balance hormone levels.
- Natural remedies: Many women turn to natural remedies for PCOS, such as herbal supplements like spearmint tea, cinnamon, and saw palmetto, to manage symptoms. While these remedies may provide relief, it’s important to consult with your healthcare provider before starting any new treatment.
Some Frequently Asked Questions about PCOS
Is PCOS an autoimmune disease?
No, PCOS is not classified as an autoimmune disease. However, it does share some overlapping symptoms with autoimmune conditions, which can sometimes lead to confusion.
Can PCOS be treated naturally?
While there is no cure for PCOS, natural remedies and lifestyle changes can effectively manage symptoms. Weight management, regular exercise, and specific supplements can make a significant difference.
PCOS vs. Endometriosis: What’s the Difference?
Both PCOS and endometriosis affect the reproductive system but in different ways. PCOS, Polycystic Ovarian Syndrome is primarily a hormonal disorder with symptoms like irregular periods and excess hair growth. Endometriosis involves the growth of endometrial tissue outside the uterus, leading to painful periods and other complications.
Will a hysterectomy cure PCOS?
A hysterectomy is not a cure for PCOS. While it may relieve certain symptoms, such as heavy bleeding, it does not address the hormonal imbalances at the root of PCOS.
It’s important to note that PCOS is a complex condition that affects every woman differently, but with the right care, it’s possible to manage its symptoms and live a healthy life.
From medications to natural remedies, there are numerous ways to take control of your health. Stay informed, and remember that you’re not alone in this journey.