Living with Polycystic Ovary Syndrome (PCOS) can feel like a never-ending cycle of trying, failing, and trying again. For many women, even after finally getting a diagnosis, the struggle doesn’t stop there. Medications that are supposed to help often fall short, leaving you feeling frustrated and back to square one. If this sounds familiar, you’re not alone.
In this article, we spoke to five Nigerian women who have been through it all—misdiagnoses, endless tests, and treatments that just didn’t work out. They’re sharing what they’ve dropped, what’s working for them now, and the alternative treatments that have helped them reclaim control of their bodies.
Ibukun, 29
After being diagnosed with PCOS in 2016, her first line of treatment was oral contraceptives. “I’ve never had regular periods, but once I started taking one pill every day at the same time, I got my period.”
While they worked to regulate her cycle, she didn’t notice the other ways the contraceptives were affecting her life until recently. “I had mood swings every now and then. Sometimes, I didn’t know which version of myself I was going to get.”
Despite their effectiveness, her gynaecologist switched her to Metformin, which she says made her body smaller but left her with constant headaches. “I eventually had to stop using it when the headaches got too bad.”
That’s when she met a female gynaecologist who reassured her that she could live without regular periods until she was ready to have kids. “This made the decision to stay off treatments very easy. But I won’t lie; I missed the weight loss that came with using Metformin, but I just couldn’t deal with the recurring headaches.”
Since then, she’s tried many things—so many that she’s lost count. “I use supplements on and off, but they delay my periods. I sometimes find my way back to good old contraceptives and thug it out for 28 days. I don’t do it often, maybe once or twice a year.”
Although she’s attempted dietary changes, she hasn’t been consistent. “So far, my hack has been being physically active. It might not give me my period, but it helps ease the fatigue that’s at the center of my PCOS symptoms.”
She believes that PCOS care should go beyond just focusing on reproduction. “Every body is different, so I’d say, explore and find what works for you, then stick with it. You just have to be very patient and never compromise on physical activity. Also, please love your body.”
Jo, 27
After being diagnosed with PCOS, Jo’s first treatment was Evening Primrose. “It did absolutely nothing for me,” she says, reflecting on her experience.
Later, she was prescribed Metformin, which turned out to be a nightmare. “I experienced nausea, diarrhea, and stomach pain. The doctor never mentioned I needed to take it with food, so I spent a week suffering on an empty stomach until I found out online that I should have been taking it with meals to minimize the side effects.”
Despite making that adjustment, the nausea and stomach issues persisted, and she still didn’t get her periods. “One day, I was venting to my partner about my frustration, and after analyzing my life before and after Metformin, I decided to quit. Believe me, I felt relieved.”
Now, she’s looking to try new medications, but if those don’t work out, she plans to switch to supplements and weight lifting, alongside her Pilates and yoga routines. “I’ve greatly cut down on red meat, alcohol, processed foods, carbonated drinks, and fast food. I eat more home-cooked meals, fish, and fruits these days.”
In addition to her dietary changes, she incorporates meditation and walking into her routine. “This has helped me a lot. I can’t advise anyone living with PCOS because it’s different for everyone, but I’m slowly putting together a routine that works for me. The core principle is to minimize stress and listen to my body.”
Ellie, 23
Like Ibukun and Jo, Ellie was also prescribed birth control pills at the point of diagnosis. “I gained a lot of weight. It affected my libido and my mental health.
The weight gain made her conscious and worsened her emotional stress. “I continued for a few months before I realised that I felt worse than I did before I started them so I stopped.”
She has not tried any other meds but uses alternative treatments often. “Adding cloves to my tea helps with regulating my periods, but that’s all I do.”
Rara, 26
Like Ellie, the first treatment she tried was birth control pills. “I experienced a lot of nausea, and since I was a teenager at the time, I ended up losing a lot of weight. My face broke out terribly too!”
When she realized the pimples were getting worse, she asked her doctor to switch her treatment. “Thankfully, I didn’t have any other major side effects.”
Though she felt relieved when she stopped the medication, she still worried about how her PCOS would manifest. “Some days are really bad, but it’s not totally unbearable.”
Now, she manages her symptoms with magnesium and evening primrose oil, and she’s also added lavender tea to her routine. “I’ve learned a lot more about how PCOS manifests, and sometimes addressing the individual symptoms works better for me than trying to tackle everything at once.”
Her advice to others? “Explore your options, be kind to yourself, and just keep trying.”
Tiff, 30
When she was first diagnosed earlier this year, her treatment journey began with a medication she can’t even recall, which was meant to induce ovulation. After that, she was placed on birth control for three months, followed by Metformin and Hyponidd for an additional six months. “This treatment plan completely threw my hormones off balance. I became erratic and unpredictable.”
Although she did get her period as expected and her metabolism improved, her overall life felt like a mess. After completing the prescribed timeframe, she decided to stop the medications and began searching for alternatives that would actually work for her.
“I felt like myself again. I was happy, my energy returned, and I could focus on work.” Through research and feedback from other women, she started taking various supplements, including Berberine, Myo-inositol, Vitamin D, Magnesium, L-carnitine, Zinc, COQ10, and Spearmint Tea. “I’ve tried it all. So far, Chia water works best for me with minimal side effects. My least favorites were Berberine, Myo-inositol, and Spearmint Tea.”
She’s also made significant dietary changes, reducing her alcohol intake and increasing her consumption of protein, whole grains, and fruits. “I’d say anyone living with PCOS needs to be patient through the trials. It’s the only way to find what truly helps ease your symptoms.”
READ: Everything You Need To Know About PCOS In 2024
Important note from Dr. Islamiat Gbajumo, in-house Doctor, Clafiya.
“While the article discusses various medications and supplements, it is crucial for individuals to consult with their gynecologist or healthcare provider before starting any new treatment regimen. Each person’s situation is unique, and what works for one individual may not necessarily be effective for another. In some cases, self-medicating based on others’ experiences can lead to complications or worsen symptoms.
Patients should feel empowered to discuss any information they find online with their healthcare provider, who can help determine the most appropriate course of action tailored to their specific needs. Ultimately, effective management of PCOS requires a collaborative approach between the patient and their medical team.”
With these stories shared by these women, it’s important to note that living with Polycystic Ovary Syndrome (PCOS) is not just about managing symptoms; it’s also about finding what truly resonates with your body. By sharing their experiences, these women hope to inspire others to explore various treatments, including natural remedies and the best supplements for PCOS management. Embracing different approaches—whether it’s lifestyle changes, alternative therapies, or simply listening to your body—can lead to meaningful improvements. This underscores the importance of personalizing your treatment journey.
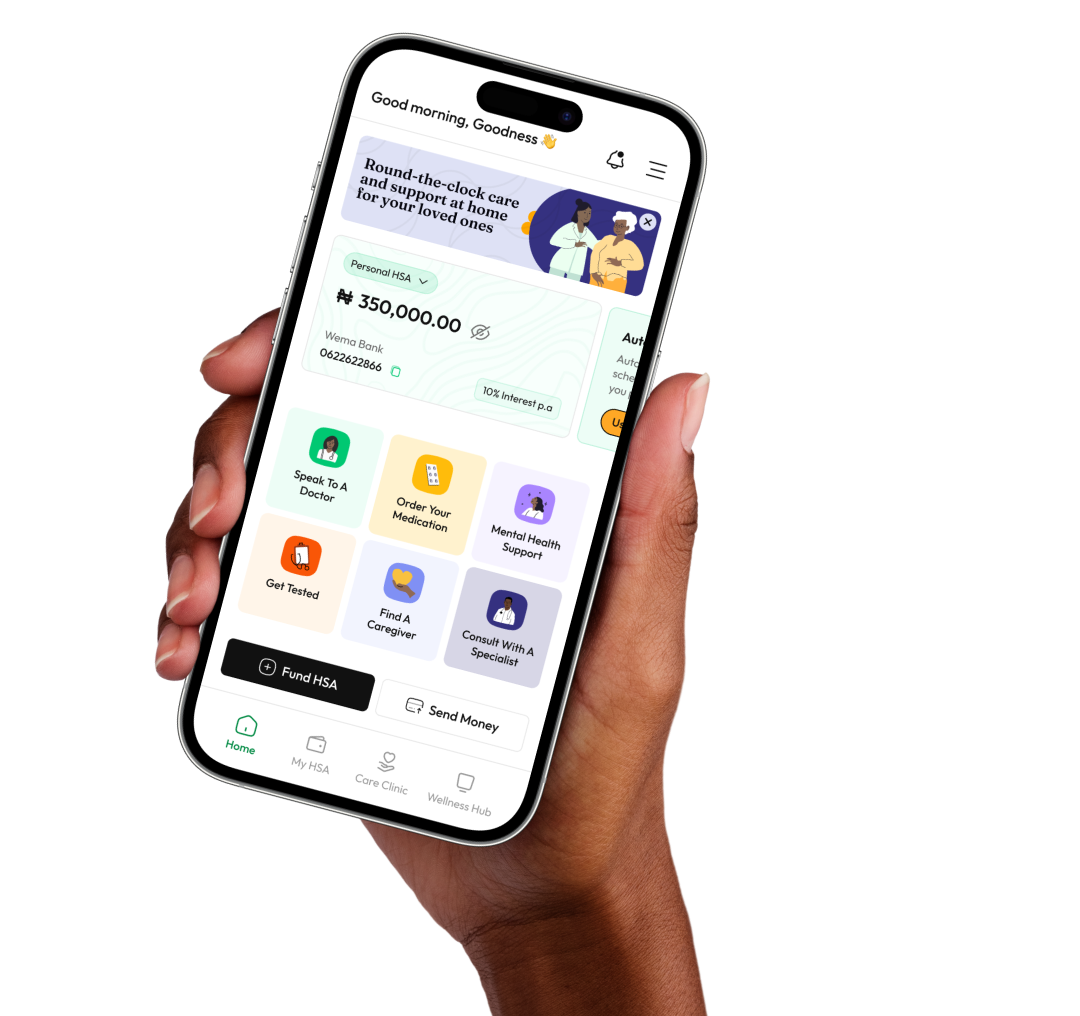
If you’re looking for personalized support tailored to your unique needs, connect with our team of doctors, pharmacists, and dieticians who are dedicated to helping you navigate this journey.
And, for more resources and insights specifically designed for Nigerian women, subscribe to our newsletter.